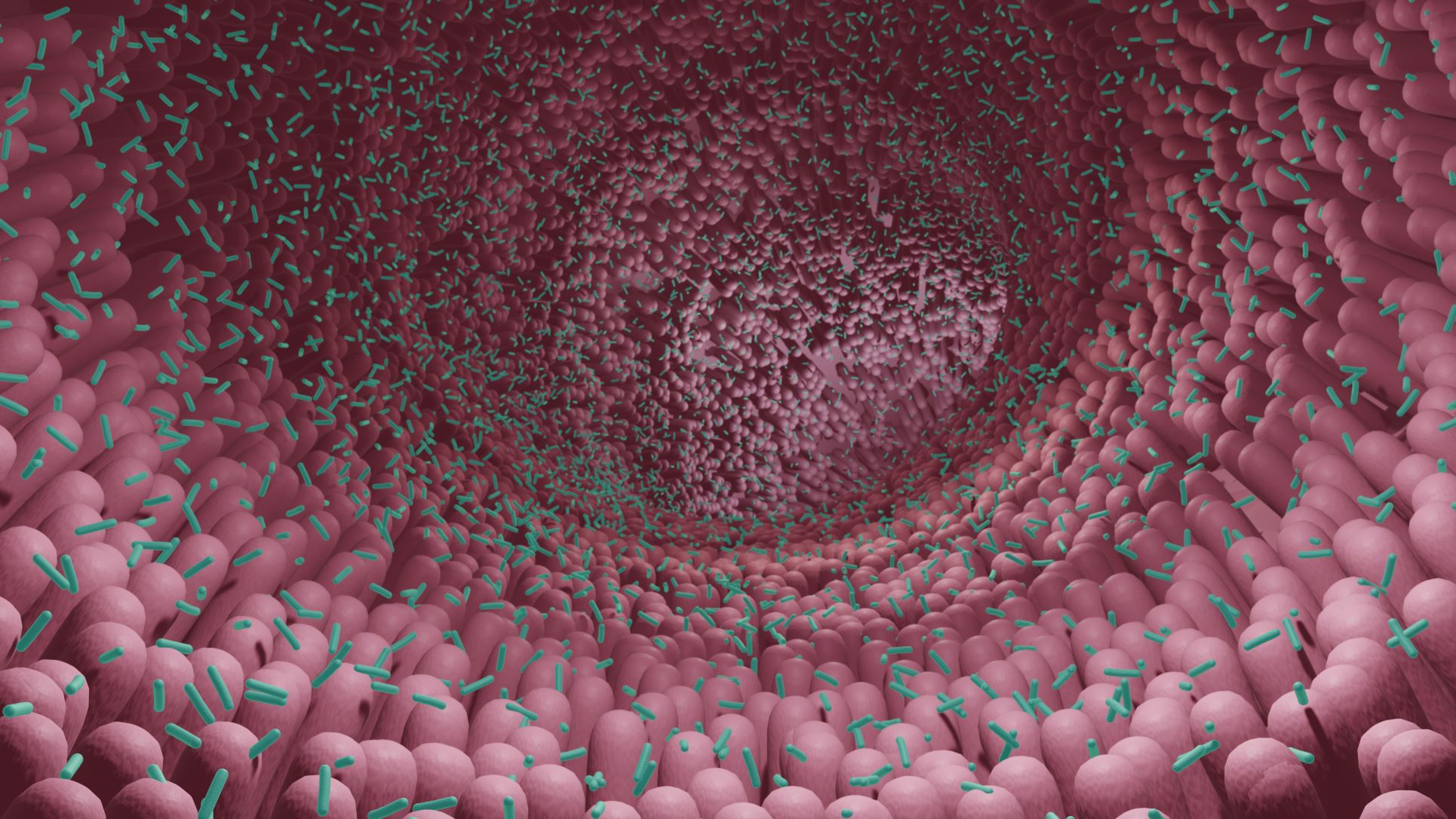
The human microbiome consists of all microorganisms found inside and on the body together with all “nonliving” components, such as genes (DNA/RNA). The microbiome is not precisely defined. In the past, it was defined as the collective genome of all the microorganisms inhabiting a specific organ. More recently though the definition has broadened to include both the microbiota, and its “theatre of activity”.1 This includes genes, structural elements (lipids, proteins, etc.) and metabolites.
Microbiota is defined as all the living members of the microbiome and composed of various types of microorganisms. Microorganisms are bacteria, fungi, archaea and small protists. Viruses, while usually not considered “living”, are still sometimes included in the microbiota. Viruses are however definitely part of the microbiome.
Different parts of the body host different compositions of the microbiome and of the microbiota. The majority of inhabitants in the human microbiota are bacteria but the composition of the bacteria differs between locations. The main function of the microbiome and microbiota can also differ but there are some common functions. One shared trait is when there is a balance between the different bacterial species and strains, the microbiota supports a healthy state. On the other hand, a dysbiosis in the microbiota composition can lead to a disruption of bodily functions resulting in varying symptoms and even the development of diseases. Dysbiosis is a state when the different bacteria don’t thrive, or when a few species are dominating the microbiota and limiting others.
The majority of all bacteria we carry in and on the human body is located in the gastrointestinal tract. In fact, up to 95% of all bodily bacteria is found in the gut.2 The gut microbiota plays a central role in maintaining and promoting overall health. It performs numerous functions, such as maintaining and strengthening the gut barrier, and supporting digestion and a well-functioning immune system. In recent years, more data showing a connection between the gut and the brain, the “gut-brain axis”, has also evolved.
Crucial for maintaining health, the gut barrier is the surface separating the inside of the intestines and the inner body. If this barrier is disrupted, also called “leaky gut”, everything from low-grade inflammation to severe complications such as sepsis or organ failure can occur. The bacteria and their composition are therefore one of the most important and fundamental aspects of staying healthy. With age, the composition and richness of the gut microbiota changes, and with it, the risk for leakage over the intestinal wall and low-grade inflammation increases. This has been coupled with many of the most common diseases today, such as cardiovascular events, osteoporosis, diabetes type II and even cancer. Read more about the functions of the gut microbiota here.
 Skin Microbiota
Skin MicrobiotaBeing the largest organ of the human body, our skin can be seen as the body’s shield, protecting its more or less sterile interior from the highly microbial outer environment. Acting as a first line of defense, skin plays a fundamental factor of health maintenance. Skin’s surface is covered with a highly active and diverse microbiota, which has been found to be of utmost importance for everything from wound healing to skin diseases.
Skin microbiota consists of both bacteria (ex Corynebacterium, Propiobacterium, Cutibacterium and Staphylococcus), fungi, viruses and archaea. In a healthy state, these microorganisms live in perfect harmony and assist in maintaining a healthy skin barrier. It is relatively stable over time, except from specific life changes which affect its composition, such as childhood, puberty, pregnancy and aging. The skin microbiota can also be affected by external factors, such as stress, sun-exposure, personal hygiene, and lifestyle. These changes can lead to a negative shift in the composition, creating a dysbiosis, with a potential outcome of pathological skin conditions such as dermatitis, psoriasis and acne.3
Across different areas of our skin there exist different skin types. And with them, the composition of the microbiota is also different. This means there are varying microorganism types present in dry, moist and oilier parts of the skin. The microbes in the skin microbiota are unevenly distributed across the total surface. Even though the microbiota is mostly found in the outer part of the skin, the epidermis, there are also microorganisms present in underlying layers, such as the dermis and underlying fat tissue. This aspect is believed to be of upmost importance when investigating the impact of the microbiota in severe skin diseases.4
Oral microbiota consists of several hundred different bacterial species. Important not only for oral cavity health, it matters for overall systemic health. The microbiota covers all surfaces in the oral cavity, from the soft tissue to the teeth where it forms a dental biofilm. There is also a diverse microbiota in the saliva, up to 109 microorganisms per milliliter.
One of the most prevalent bacterial species is streptococci, colonizing both hard and soft tissues. Like skin microbiota, oral microbiota changes with age, the first obvious change being when an infant develops teeth. The next remarkable change in the oral microbiome composition occurs during puberty, in association with a change in hormonal levels. Adulthood appears to be rather stable if good oral hygiene is maintained. With increasing age, the composition may shift, mostly coupled with a lower saliva production, intake of various medicines and/or dental restorations.
As mentioned, microbiota covering hard tissues creates a biofilm, also commonly known as plaque. This biofilm changes rapidly, in a process called succession. At first, the biofilm is dominated by streptococci, but if left untreated, rapidly evolves to an anaerobic community of Gram-negative bacteria which can cause oral diseases such as gingivitis and periodontitis. Once established, these biofilms are fairly resistant to antibacterial substances. The formation of biofilm, or plaque, is the main motivation for practicing a daily dental routine that includes mechanical cleaning with a toothbrush coupled with flossing. This care is strongly recommended to maintain a healthy oral microbiota and overall health status.4
The human respiratory tract spans all the way from the nostrils to the lung alveoli. The respiratory microbiota is thus strongly related to the microbiota of the oral cavity, but also with gut microbiota. Changes to oral microbiota, especially caused by certain bacteria, have been connected to the development of acute otitis media (ear infections) and upper respiratory tract infections. The connection between gut microbiota and the respiratory system is sometimes called the “gut-lung axis”.
Microorganisms found in the respiratory tract are not as diverse as in oral or gut microbiota but are instead quite niche-specific. They work as gatekeepers, acting to prevent invading pathogens to colonize and enter the cells, causing infection and disease. For example, a common cold is caused by invading viruses which enter the cells lining the respiratory barrier and then begin to replicate. When it does, it can set off a cascade of immune related events.
Respiratory tract microbiota is more concentrated in the upper areas. For an invading respiratory pathogen, colonization in the upper respiratory tract is important before it can spread to the lower respiratory tract. To prevent such infection, a strong microbiota resistance towards the pathogens is important.
There are many host and environmental factors that influence the respiratory microbiota composition, especially during childhood when the balance between different bacteria and microorganisms has not yet settled. Use of antibiotics, especially in young children, has a great influence on this balance, consequently creating increased risk for respiratory infections. Also, mode of delivery, daycare environment, diet, smoking and vaccinations can also affect the composition. Changes or dysbiosis in the microbiota composition, again, especially in the upper respiratory tract, increase the risk of both bacterial and viral infections.5
In men, urogenital microbiota is predominantly found in the distal urethra and includes bacteria species also commonly found in skin microbiota. For women, the microbiota is found in the distal urethra and vagina, with the vaginal composition being the main target of interest. The upper organs of the urogenital areas in both genders are considered more or less sterile, whereas changes to the lower area have shown a connection to increased risk for different diseases, such as urinary infections, bladder cancer, bacterial vaginosis and also HIV.4,6
Vaginal microbiota is a complex system influenced both by genes, environmental factors and ethnicity. The main bacterial species inhabiting the vaginal tract are different lactobacilli. Healthy vaginal microbiota contributes to continued health by decreasing the risk of infections and inflammation. It has also shown upmost importance for a normal pregnancy and reduced risk of preterm delivery. The vaginal microbiota are also the first external bacteria that colonizes the vaginally born baby.4
References
1.Berg et al, 2020 2.APC Ireland 3.Byrd et al, 2018 4.Egert et al, 2016 5.Ho Man et al, 2017 6.NIH

Bacteria are classified into different groups according to traits. Find out how you can differentiate between the bacteria.
Gut microbiota is fundamental for maintaining health and preventing several common complications and diseases. The human body...
We know probiotics are living bacteria, but in reality, they’re more. Find out what it takes to be a probiotic.