Gut microbiota is fundamental for maintaining health and preventing several common complications and diseases. The human body hosts several millions of different bacteria, with most of them found in the gut. In this text, the gut is referred to as the small and large intestines, from the duodenum all the way to rectum.
The bacteria found along the intestine varies a lot, both in number and in species composition, partly depending on the bacterial sensitivity towards oxygen. The less sensitive bacteria, such as many lactobacilli, can be found in the upper area of the intestine. Bacteria more sensitive to oxygen, such as bifidobacteria, are found mainly in the lower small intestine and the large intestine.
A microbiota where the bacteria are living in harmony with one another is of course preferred from a health perspective. However, we often hear about dysbiosis, when the different bacteria don’t thrive together or where a few species are dominating the group. But why is this so important? The main activity of the gut microbiota can be categorized into four main functions;
The composition of the gut microbiota is important for supporting all these functions and staying healthy. A dysbiotic microbiota could potentially affect one or several of these functions in a negative manner. Let’s explore the functions and their importance one by one.
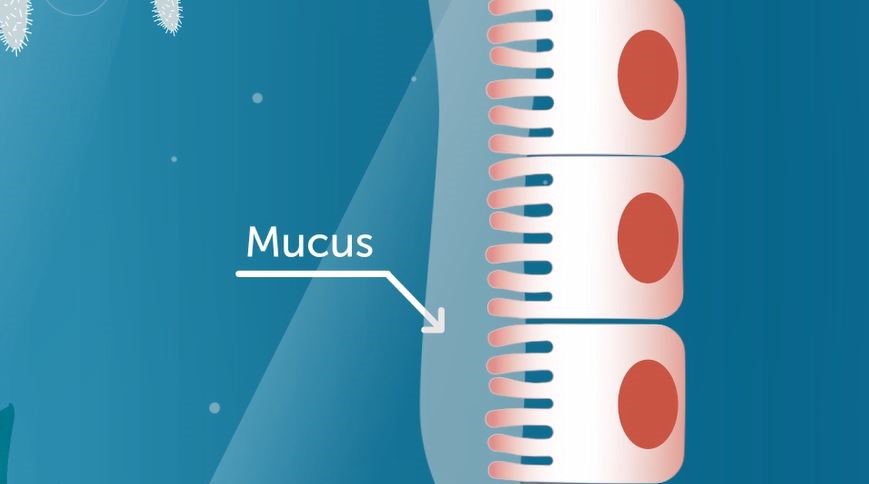
The gut barrier is made up of a single cell layer of epithelial cells, or “enterocytes”, and a thick mucus layer. The mucus layer covers the cells on the inside, in the intestinal lumen. There are multiple layers of mucus covering the inside of the stomach and the large intestine, but only one layer of mucus in the small intestine. The mucus layer is a first line of defense for invading pathogens, preventing them from crossing the intestinal barrier and into the blood stream.
Some bacteria can bind either to the mucus layer(s) or even pass through the mucus and bind directly to the intestinal cells. The gut bacteria can promote the production of mucins that make up the mucus layer, making it even stronger and harder for pathogens to penetrate.
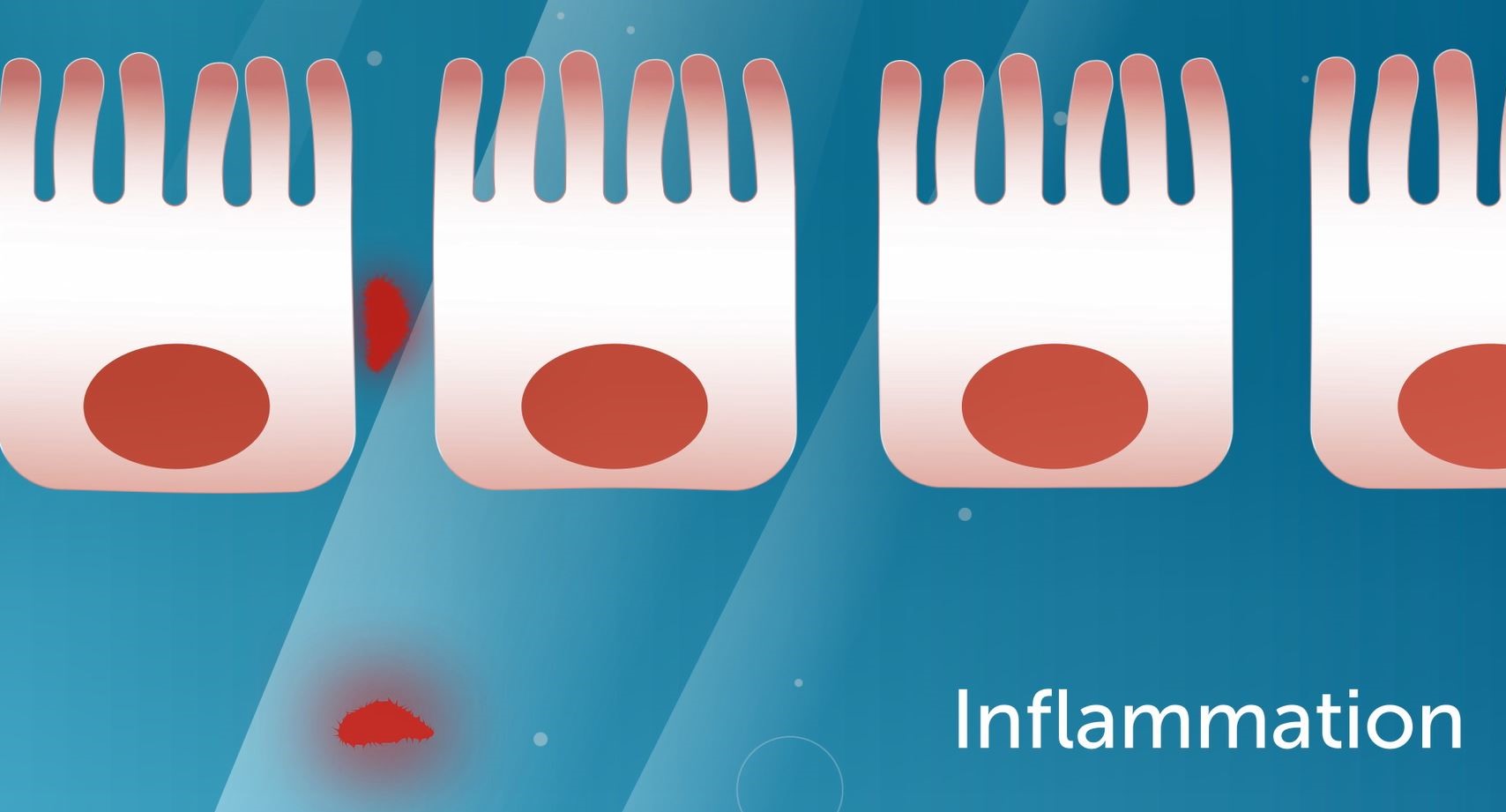
The gut bacteria can also affect the intestinal cells and the structure found between the cells, also known as “tight junctions”. These act to hold the intestinal cells tightly together. By improving the tight junctions, a stronger gut barrier is promoted. This decreases the risk for translocation (or, “leaky gut”). A dysfunctional gut barrier has been associated both with several pro-inflammatory states, the development of osteoporosis as well as to common gastrointestinal symptoms such as those found in IBS (Irritable bowel syndrome).1 More about the possible benefit of probiotics and their effect on gastrointestinal symptoms can be found here.
The gut bacteria are responsible for degrading and fermenting non-digestible food components, such as dietary fibers. While doing so, short chain fatty acids (SCFA) are formed, as well as free amino acids and other nutrients that can be used by other bacteria. The SCFA are important for metabolism as they, among many things, are part of the regulation of appetite and can affect cardio-metabolic health.
They are also crucial for the health of the intestinal cells in the large intestine , since SCFA are the primary energy source for the cells.2 The gut microbiota also produces some of the essential vitamins, such as vitamin K and B12.3 Certain bacteria have been found to affect the absorption of nutrients in a positive manner. For example, the Lactiplantibacillus plantarum 299v has been shown to positively affect the absorption of iron in the upper small intestine.4 More about the absorption of iron can be found here.
More than 70% of immune cells are regulated from the gastrointestinal tract. Therefore, it's not hard to understand the importance of gut microbiota to maintain a healthy immune function and regulation. There is also a direct communication between the gut bacteria and the immune cells. The regulation of the immune system is also connected to the gut barrier.
If the gut barrier is impaired, a leaky gut will allow substances into the blood stream which can cause low grade inflammation or disease. On the other hand, a strong and resilient gut microbiota can promote a healthy immune function which may lower the risk of acquiring infections and diseases. Many autoimmune diseases have also been connected to the gut microbiota composition, and certain probiotic strains have been shown to decrease inflammation.5-7 Read more about probiotics and how they influence the immune system here.
The gut-brain axis is often used to describe the bi-directional communication between the gut and the central nervous system. The gut microbiota can affect signaling molecules and produce metabolites which affect brain functions in different ways. For example, the hormone serotonin that makes us feel happy is produced in the gastrointestinal tract.
There are also more long-term regulations, such as affecting immune cells that are directly responsible for a certain neurocognitive reaction. One such reaction can be stress. Numerous studies indicate that the gut microbiota and probiotic bacteria may positively affect memory, cognition, depression and other functions strongly associated with neurocognitive diseases.1
References
1.Gwak et al, 2021 2.Canfora et al, 2015 3.Byrne et al, 2015 4.Hoppe et al, 2017 5.Yoo et al, 2020 6.Rask et al, 2013 7.Håkansson et al, 2019

Bacteria are classified into different groups according to traits. Find out how you can differentiate between the bacteria.
We know probiotics are living bacteria, but in reality, they’re more. Find out what it takes to be a probiotic.
The human microbiome consists of all microorganisms found inside and on the body together with all “nonliving” components, such...